Medical Drug Rebate System (MDRS)
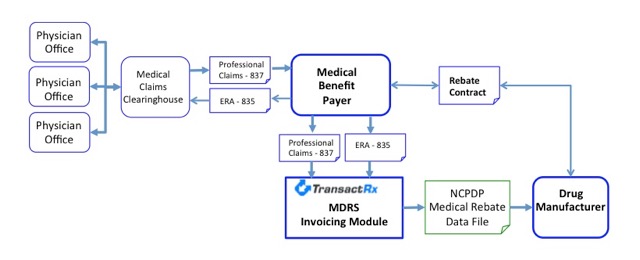
The TransactRx Medical Drug Rebate System (MDRS) is a complete system supporting all functionality required to load Drug Manufacturer rebate contract details, import drug administration information from pre and post adjudication professional medical claims data, create medical drug rebate invoices and transmit them to the appropriate manufacturer. The MDRS is based on industry standard data formats and can be implemented by a Medical Benefit Plan/Payer with very little IT resources and in a short amount of time.
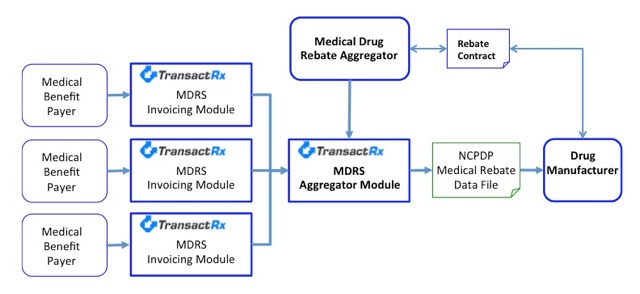
The TransactRx MDRS platform is made up of two components; the MDRS Invoicing Module and the MDRS Aggregator Module. The MDRS Invoicing Module is implemented by a Payer that has its own Medical Drug Rebate contracts or is contracted with an aggregator that owns the rebate contracts. The MDRS Aggregator Module is implemented by an organization that owns Medicare Drug Rebate contracts and acts as an aggregation point for sub-contracted entities to submit their rebate invoices or drug administration information and then combines data into consolidated rebate invoices for transmittal to manufacturers.
TransactRx MDRS Invoicing Module
The TransactRx MDRS Invoicing Module is implemented as a service with nothing required to be physically deployed at the payer site. The interface to the MDRS invoicing module can be deployed using standard X12 837 professional claims and X12 835 electronic remittance advice data records. At the request of the payer the interface can use mutually agreed to proprietary data feeds as well. The MDRS Invoicing Module can be implemented as a complete solution for payers with their own rebate contracts or as a method of transmitting data to a rebate aggregator.
Functional Specifications of the MDRS Invoicing Module include:
- Payer contract information is loaded in MDRS Invoicing Module:
- Drug products covered under the contracts.
- Payer and Patient payment requirements.
- All other rules per each manufacturer drug product.
- Invoicing rules and formats are configured.
- Payer implements a data feed to the MDRS Invoicing Module:
- Copies of all 837 claim records for an invoicing period.
- Copies of all 835 electronic remittance records associated with claims for the invoicing period.
- SFTP or any other data transfer protocol is supported.
- No changes to physician office claims submission are required:
- Physician Offices submit standard professional claims with usual HCPC codes for drug products. For HCPCS that represent more than one drug product the physician offices submit the NDC code for the specific drug administered. It is NOT necessary for the claims to include NDC based quantities or units of measure.
- The professional claims are submitted as usual through the current Medical Claims Clearinghouses to the Payer adjudication system. The claims are adjudicated and electronic remittance advice files are returned as usual.
- MDRS Invoicing Module Processing:
- 837 claim data and 835 remittance file data is imported into the MDRS data repository.
- Data for an invoicing period is processed against the contract details configured for the payer and manufacturers.
- NCPDP Medical Rebate Data Submission files are created and transmitted to manufacturers.
- Proprietary data submission formats can be supported if required.
- Payer Rebate Invoicing is stored and available for review by Payer.
TransactRx MDRS Aggregator Module
The TransactRx MDRS Aggregator Module is deployed as a service with nothing required to be physically implemented at the Rebate Aggregator site. The MDRS Aggregator Module can receive data from the MDRS Invoicing Modules implemented by various payers or from any other system capable of implementing a data feed to the Aggregator Module. The MDRS Aggregator Module supports all the functionality to load and manage manufacturer rebate contracts for any number of drugs.
Functional Specifications of the MDRS Aggregator Module include:
- Rebate contract information is loaded in MDRS Aggregator Module:
- Drug products covered under the contracts.
- Payer and Patient payment requirements.
- All other rules per each manufacturer drug product.
- Invoicing rules and formats are configured.
- Data feeds from the MDRS Invoicing Modules and other Payer data creation systems are deployed:
- Plug and Play interface to the MDRS Invoicing Modules at submitting Payers.
- SFTP or any other data transfer protocol is supported from non MDRS submitters.
- MDRS Aggregator Module Processing:
- Submitting payer data from all payers is imported into the MDRS data repository.
- Data for an invoicing period is processed against the contract details configured for the payer and manufacturers.
- NCPDP Medical Rebate Data Submission files are created and transmitted to manufacturers.
- Proprietary data submission formats can be supported if required.
- Rebate Payment Posting and Distribution:
- Payments from manufacturers are posted against invoices in the MDRS Aggregator Module.
- Individual Payer rebate amounts are calculated.
- Explanation of Payment reports can be generated by the MDRS Aggregator Module to distribute to submitting payers in support of rebate payments.